Mrs. Afreen is a 28-year-old pregnant woman. She was close to giving birth when she went to the hospital. She had a worrying complaint: she wasn’t feeling her baby move as much as usual. She also experienced passage of blood clots, another alarming symptom.
During the hospital examination, her baby’s heart rate dropped, indicating a possible case of fetal distress. The healthcare team had to make a quick and important decision. They decided to do an emergency C-section to protect the mother and her baby.
What is Fetal Distress?
Fetal distress refers to signs before and during childbirth indicating that the baby is not doing well. A lack of oxygen often causes it and can be life-threatening if not treated promptly. Common signs include:
- Decreased or absent fetal movements
- Irregular or low fetal heart rate
- Blood or fluid discharge
- High or low levels of amniotic fluid
In this case, the two major symptoms — reduced baby movement and blood clots — were red flags that required immediate action.
Initial Medical Evaluation and Vital Signs
Upon arrival at the hospital, the medical team performed a thorough general and systemic examination. Here are the patient’s vital signs:
- Temperature: 98.4°F (normal)
- Pulse Rate: 110 beats per minute (slightly high, possibly due to stress)
- SpO2 (Oxygen Saturation): 98% (normal)
- Blood Pressure: 130/90 mmHg (borderline high)
- Capillary Blood Glucose (CBG): 74 mg/dL (slightly low)
Mrs. Afreen was conscious, alert, and stable at the time of examination. Her heart, lungs, and nervous system showed no significant abnormalities.
However, the fetal heart rate began to drop, confirming the suspicion of fetal distress. This critical situation required an emergency Lower Segment Cesarean Section (LSCS) to deliver the baby safely.
What Is an LSCS and Why Is It Done?
A Lower Segment Cesarean Section (LSCS) is the most common type of cesarean delivery. It involves making a horizontal cut in the lower part of the uterus. This approach has fewer complications and allows for better healing compared to classical vertical incisions.
Emergency LSCS is performed when the baby or mother is in immediate danger. In Mrs. Afreen’s case, the decline in fetal heart rate confirmed that the baby needed to be delivered without delay.
Detailed Step-by-Step Procedure of the Surgery
1. Anesthesia and Patient Positioning
- Mrs. Afreen was given spinal anesthesia, which numbed her body from the waist down while keeping her conscious.
- She was placed in a supine position (flat on her back).
- The surgical site was thoroughly cleaned and draped to maintain sterility.
2. Opening the Abdomen and Uterus
- The surgeon made an incision in the abdominal wall and carefully separated layers to reach the uterus.
- The peritoneum (a lining inside the abdominal cavity) was opened.
- The utero-vesical fold (the space between the uterus and bladder) was gently separated. This helped to show the lower part of the uterus.
3. Delivering the Baby
- The lower segment of the uterus was found to be thick, which made the delivery a bit challenging.
- They clamped and cut the umbilical cord.
- The nurse immediately handed the baby to the pediatrician for examination and postnatal care.
4. Stem Cell Collection
Researchers collected and saved stem cells from the umbilical cord. You can use them later to treat different health issues.
5. Completing the Procedure
- The placenta and membranes were completely removed.
- The surgeon closed the uterus with 1-Vicryl interlocking sutures to ensure strong, secure healing.
- The surgical team checked for bleeding (haemostasis) and confirmed everything was in order.
- The doctors examined the ovaries and fallopian tubes on both sides and found them to be healthy.
- We verified the instrument and pad count to avoid any retention.
- The patient’s urine output was normal.
- Finally, we performed vaginal cleaning (toileting) to reduce the risk of infection.
Outcome and Recovery
The surgery was completed, and both mother and baby were healthy and stable after the operation. The pediatrician said the baby was doing well. The medical team then moved the mother to the recovery room for care after surgery.
Post-Operative Care for Mother:
- Monitoring vital signs (blood pressure, pulse, temperature)
- Managing pain with prescribed medications
- Ensuring proper wound healing
- Encouraging early breastfeeding and bonding
- Helping the mother walk after 12–24 hours to prevent blood clots
Postnatal Care for Baby:
- Pediatrician’s evaluation
- Monitoring feeding and reflexes
- Checking for any signs of infection or breathing issues
- Safe preservation of stem cells for future use
Why Timely Medical Attention Matters
Many women may think decreased fetal movement is “normal,” especially in the last stages of pregnancy. However, any sudden change in movement patterns must be taken seriously.
In this case, Mrs. Afreen acted quickly by visiting the hospital on time. This fast action:
- Saved her baby’s life
- Prevented complications like brain damage due to oxygen shortage
- Avoided serious maternal issues like uterine rupture or infection
Health Tips for Pregnant Women
- Always monitor baby movements, especially in the third trimester.
- Attend all prenatal checkups as advised.
- Report any abnormal symptoms like bleeding, severe pain, or reduced fetal activity.
- Eat a balanced diet and stay hydrated.
- Discuss stem cell banking options in advance if interested.
Takeaway Message
Mrs. Afreen’s case shows that early detection of fetal distress is important. Doctors can successfully treat it with an emergency cesarean section. Her quick choice to get medical help, along with
Dr. Gowri C and the surgical team, made sure her daughter was born safely. Now, both mother and baby are doing well.
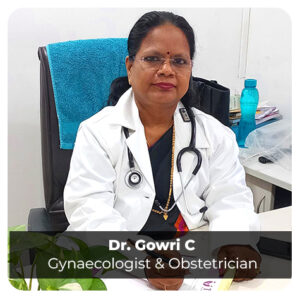
Remember, in pregnancy, time matters. Never ignore warning signs. A small choice, like going to the hospital after feeling fewer baby movements, can change everything for safety.